One of the main worries for new ostomates is the possibility of their stoma becoming infected. Infections around a stoma are rare, but can happen for various reasons so it is essential to have a good skin care regime in order to maintain healthy skin. Check your stoma and skin regularly each time you change your stoma appliance, which will help identify any new issues if they arise.
Our skin is home to millions of bacteria, fungi and viruses which compose the skin microbiota. Like those in our gut, skin micro-organisms have essential roles in protecting against invading pathogens. These micro-organisms can easily multiply when you have a stoma because the area is warm, humid and soiled. They may colonise the stoma without causing any major issues. But for those who suffer with general ill-health, diabetes or those who take immunosuppressive medications, infections are more likely to occur.
The skin around the stoma can become inflamed and irritated due to infection, yet there are other reasons for sore skin such as the stoma appliance leaking, or underlying disease. Often minor skin infections can cause red, inflamed skin surrounding the stoma. Ongoing skin irritation can cause papules (small bumps) and nodules (larger bumps) so it is wise to get your skin checked out by your Stoma Care Nurse. Irritated skin can usually be resolved by identifying the cause of any leaks and commencing stoma powders/creams/wipes/sprays to help heal and protect the damaged skin.
So, what are the signs of an infected stoma? When the skin becomes infected it can start to look inflamed and the infection tends to cause some swelling around your stoma. The skin colour often changes from a healthy pink/reddish colour, to pale, bluish purple or even black. If there is any discharge of blood or pus this is often a definitive sign of infection. Infections can also cause increased pain and discomfort. Speak to your GP if these symptoms occur as you may need a swab taking and a course of antibiotics.
Types of infections:
It is wise to be aware of the type of infections you can experience when you have a stoma. Infections of the skin tend to be either bacterial, viral or fungal. Infections of all types are miserable and can cause interference with the stoma itself and the appliance adhering to your skin.
Bacterial Infections:
Bacterial infections are the most common type of infections for those with a stoma. Any break in the peristomal skin caused by leakage, allergic contact dermatitis or other chronic skin conditions. increases the risk of infection. The most common bacterial infections are caused by staphylococcus aureus or streptococci or both entering through broken skin.
Bacterial infections are usually confirmed with a swab, so make sure you reach out to your stoma care nurse or GP if you suspect an infection. Stubborn/severe infections may need to be treated with a course of antibiotics.
- Bacterial infections can be present as a secondary infection of a surgical wound, so having stoma surgery could put you at risk of skin infections
- Bacterial infections may also cause folliculitis (inflammation of the hair follicles) or boils (hard painful lump which fills with pus).
- Impetigo – a highly contagious skin infection that often starts with red sores or blisters and leave golden brown patches
- Cellulitis – is a potentially serious bacterial skin infection which needs immediate treatment. It affects the surface skin and can make your skin painful, hot and swollen. But it can also affect the tissues underneath and can spread to your lymph nodes and bloodstream, becoming life threatening, if action is not taken. Don’t be alarmed though – this is very rare!
Fungal Infections:
Yeast (fungal) infections can occur on the skin around the stoma. These types of skin infections cause a red, raised, itchy, pimply rash. It usually improves and resolves with antifungal powder or cream. Severe yeast infections can be confirmed by skin scrapings via your Stoma Care Nurse.
- Thrush (candida fungi) – can occur at almost any area of the body, but they prefer warm, damp creases of your body such as armpits, groins, under breasts and perineum. Therefore, under a warm and moist pouch can be just the perfect condition for them to grow!
- Tinea Corporis (ringworm) – is a rash which is usually red, itchy and circular, with a clearer area in the middle. Ringworm gets the name from its appearance; no worm is actually involved!
- Pityriasis versicolor (Malassezia) – causes patches on your skin which may be lighter or darker than your normal skin
Viral infections:
Viral infections are far less common in ostomates. When they do occur, they can present challenges as they can cause interference with a stoma appliance adhering to the skin.
- Herpes zoster (shingles) and herpes simplex (cold sores) – these areas can often become infected by staphylococci and therefore should be swabbed by your GP or Stoma Care Nurse before antiviral treatment is given
- Viral Warts – warts and verrucae are small lumps on the skin causes by the virus. They appear as a small rough lump on the skin. They spread easily through skin contact and infected surfaces.
- Molluscum contagiosum – is quite unusual in ostomates. Molluscum appears as small, firm spots that have a dimple in the middle and can be very itchy. It is contagious and therefore try not to share towels and in time it will tend to clear up on its own.
Peristomal abscess:
One or more open and painful lesions can occur around the edges of the stoma, surrounded by a halo of redness. This is not uncommon with those who have suffered with Crohn’s disease in the distal bowel. Abscesses can often be treated by antibiotics from your GP and monitored by your Stoma Care Nurse.
In severe cases re-referral back to the surgeon maybe required and the ostomate may have to undergo drainage of the abscess or unroofing of the ulcer by the Surgeon.
Recommended products…

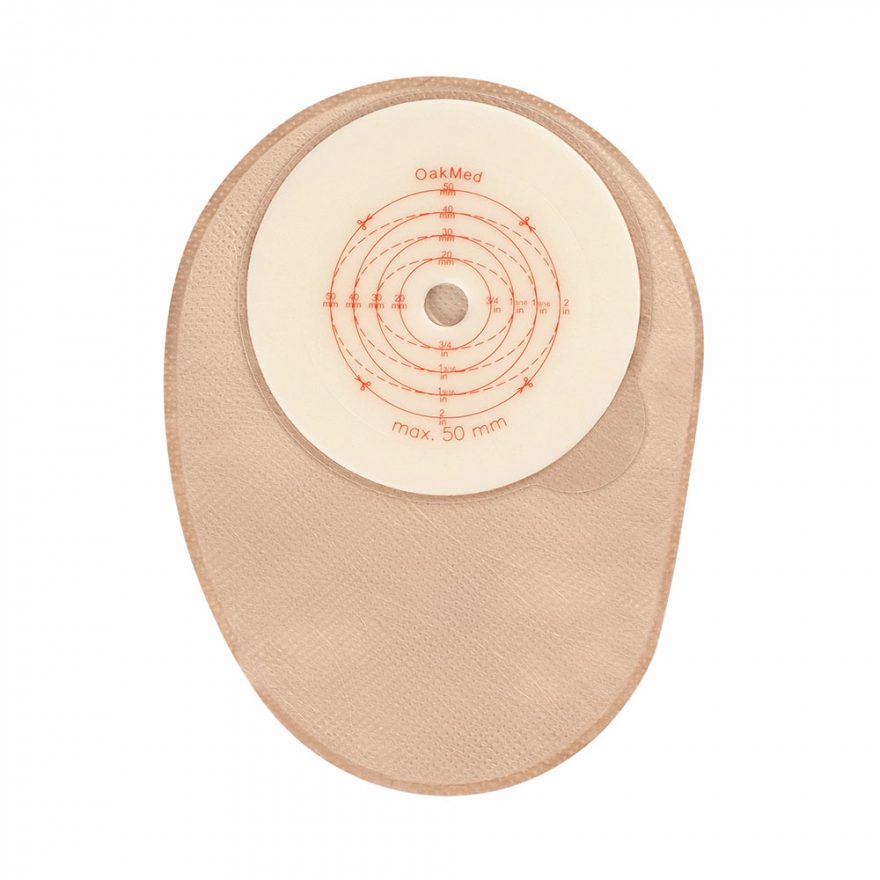
Closed Mini Alginate
View the product

